Guttmacher Institute
Nearly all abortions in Zimbabwe are clandestine, with many resulting in complications that require medical treatment. However, half of women who experience complications from unsafe abortion in Zimbabwe never receive the care they need. These findings come from a new study conducted by researchers from the University of Zimbabwe College of Health Sciences Clinical Trials Research Centre (UZCHS-CTRC), the Zimbabwe Ministry of Health and Child Care, Women’s Action Group and the Guttmacher Institute. The study provides the first comprehensive estimates of the incidence of abortion and post-abortion care in Zimbabwe. The findings are based on surveys of all health facilities in the country, as well as experts on abortion and women seeking post-abortion care – which includes treatment for complications from unsafe abortion and miscarriage – and were published in the journals PLOS ONE and BMJ Open.
Abortion in Zimbabwe is only legally permitted to save the life of the pregnant woman or in cases of rape, incest or fetal impairment. Even under these circumstances, it is extremely difficult for women to obtain legal abortions at a health facility. In 2016, there were an estimated 66,800 abortions in Zimbabwe. This translates to one of the lowest abortion rates in Sub-Saharan Africa – 18 abortions per 1,000 women of reproductive age – or roughly half the regional abortion rate for Eastern Africa, which is 34 per 1,000 women. However, virtually all abortions in Zimbabwe are clandestine and likely unsafe. Some women travel outside of Zimbabwe to obtain an abortion, such as to neighboring South Africa, where abortion is legal.
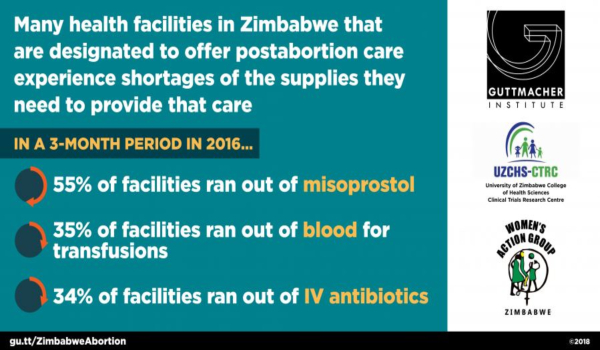
Four in 10 women in Zimbabwe who had clandestine abortions in 2016 experienced complications – such as haemorrhage and infections – that required medical treatment. However, only half of women who needed treatment received it. Many women seeking post-abortion care reported experiencing substantial delays between being seen at a health facility and receiving complete treatment, often due to lack of money, wait times, staffing shortages or inability to get complete treatment at a single facility. The vast majority of post-abortion care in Zimbabwe (85%) is provided at public health facilities. The Ministry of Health and Child Care has made efforts to expand and improve post-abortion care services in order to reduce maternal mortality, such as revising national guidelines in 2014 to make these services available at a broader range of facilities. However, ongoing economic difficulties in Zimbabwe have limited the capacity of the health system to provide post-abortion care services.
Rural women seeking post-abortion care in 2016 had twice the odds of experiencing severe complications as their urban counterparts. And adolescent women, who have the highest unmet need for contraception in Zimbabwe were more likely than women older than 30 to experience severe complications.
FULL NEWS RELEASE, 25 October 2018 ; SEE ALSO this Campaign news report with more information from this same research, 30 October 2018



