https://www.etsy.com/uk/listing/1353036717/digital-map-of-africa-colorful-…
by Amy Grossman, Ndola Prata, Sarah Jones, Lawrence Läser, Bela Ganatra, Antonella Lavelanet, Natalie Williams, Chilanga Asmani, Hayfa Elamin, Leopold Ouedraogo, Lucy Sejo Maribe, and many others
Reproductive Health. Availability of quality-assured medical abortion medicines
Vol. 20; Suppl. 1. 27 December 2024. Open access. https://doi.org/10.1186/s12978-024-01898-8
Abstract
Background: The use of medical abortion pills, either a combination of mifepristone and misoprostol, or misoprostol alone has contributed to increased safety and decreased mortality and morbidity. The availability of quality medical abortion medicines is an essential component in the provision of quality abortion care. Understanding the factors that influence the availability of medical abortion medicines is important to help in-country policymakers, program planners, and providers improve availability and use of medical abortion.
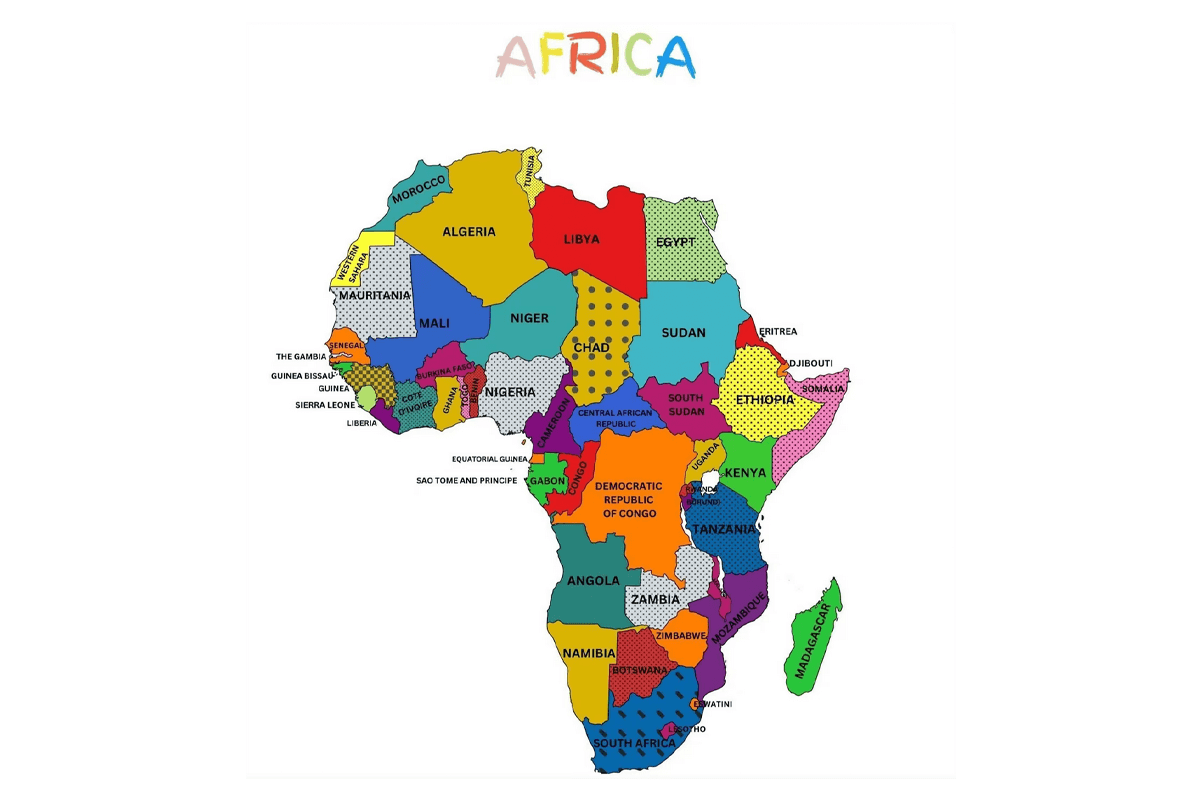
Methods: Using a national assessment protocol and an availability framework, we assessed the availability of medical abortion medicines across five elements (Registration & Quality Assurance, Policy & Financing, Procurement & Distribution, Provider Knowledge, and End-user Knowledge) in eight countries: Botswana, Burkina Faso, Central African Republic, Democratic Republic of the Congo, Eswatini, Lesotho, Namibia and Uganda between November 2020 and November 2021. The assessment included an online desk review and virtual or telephone-based key informant interviews.
Results: Registration of medical abortion medicines—misoprostol or co-packaged mifepristone and misoprostol products (combi-pack)—was established in all countries, except the Central African Republic. In Lesotho and Eswatini, the national regulatory agency is still in development and importation of Cytotec™ misoprostol is permitted for off-label use in obstetrics/gynecology. Misoprostol was included in all countries’ essential medicines lists, except Botswana. Burkina Faso and Democratic Republic of the Congo also include mifepristone on their essential medicines list and medical abortion regimens in national abortion care service and delivery guidelines. Additionally, guidelines clarified health worker roles in the provision of abortion care specific to the legal context of each country and permitted task-shifting of abortion service provision. Where guidelines did not exist, medical abortion medicines and their use were not well integrated into the public health care system. Community awareness activities on abortion rights and services have been limited in scope across the countries assessed, however, end-users’ awareness of misoprostol as a medical abortion medicine was reported.
Conclusion: The national landscape assessments identified several cross-cutting opportunities to improve availability of medical abortion medicines, including importing quality-assured medical abortion medicines; developing nationally approved abortion service and delivery guidelines that optimize healthcare worker roles; and expanding communication strategies to reach end-users and pharmacists.
Background: Recent estimates suggest that while the overall rate of unintended pregnancies has fallen, the proportion that ends in abortion has risen, largely driven by improved access to sexual and reproductive healthcare in high-income countries. The combination of mifepristone followed by misoprostol, or misoprostol alone, are World Health Organization (WHO)-recommended methods for medical abortion (MA) that offer an alternative to surgical abortion. Medical abortion has been shown to enhance autonomy, choice, and safety in abortion care. Medical abortion allows women greater control over the timing and setting of the procedure, leading to increased satisfaction and empowerment. The safety profile of medical abortion is also well-established, with low complication rates, making it a viable option for many women seeking abortion care. However, unsafe abortion—an abortion carried out by a person lacking necessary skills or in an environment that lacks minimal medical standards, or both—remains a public health challenge, particularly in low-income countries. Of the 55.7 million abortions that occurred globally each year between 2010 and 2014, about 45 percent were unsafe and nearly all took place in a developing country.
In recent years, the number of misoprostol-alone and co-packaged mifepristone and misoprostol (combi-pack) products that have been used for abortion has grown globally. Since 2014, five misoprostol and three mifepristone products and a combi-pack have been WHO prequalification (PQ)-listed, a global standard for quality assurance for pharmaceutical products. The availability of quality-assured MA medicines (WHO PQ-listed products or those approved by a Stringent Regulatory Authority (SRA)) is an essential component in the provision of quality abortion care. Understanding the factors that influence the availability of MA medicines is important to help policymakers, program planners, and providers in countries improve availability and use of quality medicines.
This paper builds upon the WHO’s landscape assessments on the availability of MA medicines, wherein “availability” means that a woman can request and receive a-quality-assured and affordable MA product or service when and where she needs it. This paper describes results from eight country assessments in Botswana, Burkina Faso, Central African Republic, Democratic Republic of the Congo, Eswatini, Lesotho, Namibia, and Uganda. The purpose of the landscape assessments was to generate evidence to support policy dialogue and policymaking that is specific to the needs of a given country, in order to improve the availability of MA medicines.
[Editor’s Note: This is a long, dense, complicated paper, with many acronyms, but it offers an important picture of the often very limited extent of the provision of abortion with pills in the national health systems of these eight countries, alongside findings showing wider access to and use of the pills outside of the health systems (often misoprostol only but slowly also combined mifepristone-misoprostol), based on a range of sources. Marge Berer]



