BMJ Sexual and Reproductive Health, Letter from Madeleine Ennis, Regina Renner, Bimbola Olure, Stephanie Begun, Wendy V Norman, Sarah Munro, 10 May 2024.
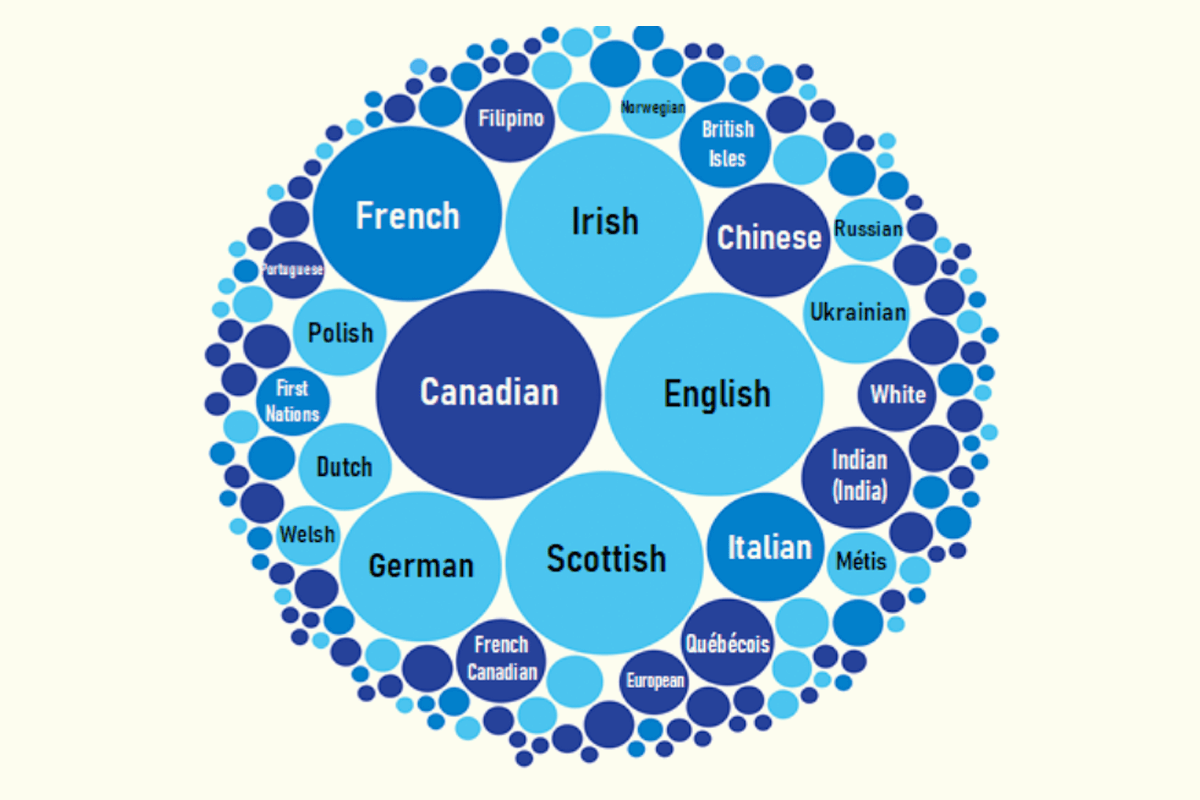
Infographic/Statistics Canada: Most common ethnic or cultural origins reported by the population, 2021
The WHO highlighted the importance of providing culturally safe, high-quality healthcare, emphasising that services should be welcoming to diverse populations, including “youth and people from sexual and gender minorities, people living with disabilities, and all groups in vulnerable and marginalised situations”.
We conducted the 2019 Canadian Abortion Provider Survey (CAPS), collecting demographics, clinical abortion practices, and stigma experiences of providers. In this research letter we present how abortion providers cared for diverse populations and the related training they had received.
Physicians, nurse practitioners and abortion service administrators who provided abortion care in 2019 were eligible to participate. To explore dimensions of care provided to diverse populations, we asked multiple-choice and open-ended questions, including: Do you provide abortion care to diverse patient populations (e.g. cultural/ethnic origins, gender/identity, etc.)? Do you adjust your abortion care to diverse patient populations? Have you ever had specific training for providing abortion care to diverse populations during your education/professional training? We present descriptive statistics analysed with R Statistical Software. We conducted a reflexive thematic analysis of the open-ended responses and organised our results in an explanatory narrative.
Of the 500 respondents who completed the CAPS survey, 356 started the Diverse Populations section and we report on the results of this sub-sample. Respondents (n=356) represented every province and territory in Canada as well as urban (59.1%) and rural (40.9%) areas. The majority of respondents self-identified as women (83.5%), clinicians (92.1%) as opposed to administrators, and having less than five years’ experience providing abortion care (65.6%).
While most clinicians reported they had not received specific training for providing care to diverse populations (91.2%), 91.8% indicated they provided care to diverse populations and almost half (47.0%) adjusted care to accommodate their patients’ needs most or all of the time. When asked which continuing training opportunities would be relevant in supporting care of diverse populations, the majority of respondents suggested web-based training (77.3%) followed by in-person training (34.1%).
Finally, participants who adjusted their care for diverse populations were given the option to provide an open-ended response to this question: Please explain how you adjust your abortion care (e.g. to specific environment, specific personnel or specific training). Our analysis of the qualitative responses from 206 participants identified five core themes (italicised below), which we summarise with sample quotations in Table 1. Participants adjusted care to the patient’s religion and/or culture, for instance by being open to managing the products of conception and/or including culturally appropriate support people. Adjusting language and communication was a core strategy participants described, through translation services, shifting the amount and speed of information shared, and offering multilingual resources with visuals.
Some participants specified that they provided gender-affirmative and trauma-informed care through use of gender-neutral language and trans-inclusive services. Other participants focused on shifting when and where services are provided including virtual health and flexible appointments. Others described relying on in-person care and closer follow-up when concerned about protocol adherence due to, for example, low literacy or English language skills. Finally, participants described offering personalised care by asking patients to share their preferences.
We identified a gap in Canada between recommendations to provide culturally safe healthcare and abortion provider-reported training opportunities to provide care to diverse populations. Most respondents reported never receiving specific training. Less than half of respondents consistently adjusted care to diverse populations, for example, by implementing trauma-informed, culturally safe and gender-affirmative practices. We were unable to assess the quality of these care practices. In order to improve and standardise provision of culturally safe care as an indicator of equitable access to high-quality abortion care, we found there is an urgent need to develop, implement and evaluate training materials specific to providing abortion care to diverse populations.
Some specific examples from Table 1
– “We serve an Indigenous population in Quebec and they occasionally request to take the fetal tissue home to bury which we will accommodate.”
– “Involvement of culturally appropriate support people (e.g., Indigenous cultural navigator/Indigenous midwife), faith-based supports (priest, imam).
“I have some patients who live far away, so I adjust to more telephone follow-up and don’t necessarily check serial hCG for those patients.”
“I work with nurses in remote First Nations communities via telehealth to increase access to abortion care.”
“…allow drop-ins and seeing people when they arrive, even if it’s late/the wrong appointment day/time.”
“…may give them the option of taking medications in hospital versus at home if they live out in the communities that are far from the ER or have poor pain tolerance and require further care.”
“I adjust amount and speed of information-sharing based on comprehension, language, education, cognitive status, mental health, expression of cultural ethical concerns.”
“Some patients request I use different terminology (i.e. not refer to their situation as a ‘pregnancy’ or avoid the term ‘fetus/baby’) for personal reasons.”
“Always using gender-neutral language, trans-inclusive assessment of services.”
“Different terms to describe procedure/anatomy/contraception, use of preferred pronouns.”
“For those with lower literacy or English language skills, I will definitely have them take the mifepristone on site. Sometimes, if I’m uncertain of their comprehension, I will have them take the misoprostol on site as well. I also follow them more closely with phone calls afterwards to ensure follow-up hCGs are done. I have created picture-rich infographics to facilitate understanding of the process.”
“I have a primarily First Nations patient base from fly-in communities. I do multiple in-person visits to ensure communication is clear and ensure medication is taken correctly as many of my patients have limited medical literacy. Our policy requires them to be near a hospital rather than returning to fly-in communities so we see them and do ultrasounds earlier to try to confirm they are safe to fly home prior to discharge.”



