by M Endler, A Lavelanet, A Cleeve, B Ganatra, R Gomperts, K Gemzell-Danielsson
BJOG: An International Journal of Obstetrics & Gynaecology 14 March 2019 (Open access)
DOI: 10.1111/1471-0528.15684
Abstract
Background: Telemedicine is increasingly being used to access abortion services.
Objective: To assess the success rate, safety, and acceptability for women and providers of medical abortion using telemedicine.
Search strategy: We searched PubMed, EMBASE, ClinicalTrials.gov, and Web of Science up until 10 November 2017.
Study criteria: We selected studies where telemedicine was used for comprehensive medical abortion services, i.e. assessment/counselling, treatment, and follow up, reporting on success rate (continuing pregnancy, complete abortion, and surgical evacuation), safety (rate of blood transfusion and hospitalisation) or acceptability (satisfaction, dissatisfaction, and recommendation of the service).
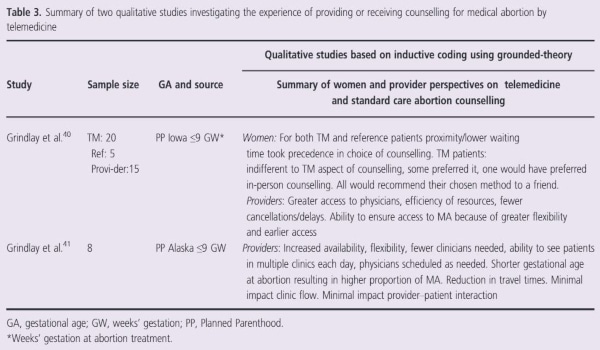
Data collection and analysis: Quantitative outcomes were summarised as a range of median rates. Qualitative data were summarised in a narrative synthesis.
Main results: Rates relevant to success rate, safety, and acceptability outcomes for women ≤10+0 weeks’ gestation (GW) ranged from 0 to 1.9% for continuing pregnancy, 93.8 to 96.4% for complete abortion, 0.9 to 19.3% for surgical evacuation, 0 to 0.7% for blood transfusion, 0.07 to 2.8% for hospitalisation, 64 to 100% for satisfaction, 0.2 to 2.3% for dissatisfaction, and 90 to 98% for recommendation of the service. Rates in studies also including women >10+0 GW ranged from 1.3 to 2.3% for continuing pregnancy, 8.5 to 20.9% for surgical evacuation, and 90 to 100% for satisfaction. Qualitative studies on acceptability showed no negative impacts for women or providers.
Conclusion: Medical abortion through telemedicine seems to be highly acceptable to women. Rates of continuing pregnancy, complete abortion, haemorrhage and hospitalisation are similar to those reported in the literature for in‐person abortion care. Surgical evacuation rates are higher. The compiled results in this review are based mostly on self‐reported data and come with several methodological limitations. To inform future policy recommendations, abortion care through telemedicine needs to be defined and research is needed on the feasibility of using TM for abortion in low‐resource settings.
LINKED ARTICLE
Commentary on this article by Daniel Grossman, ANSIRH, University of California at San Francisco, USA. 10 May 2019 at: https://doi.org/10.1111/1471-0528.15802



